This guide provides a comprehensive overview of the ABO blood group system, its importance in transfusion medicine, and applications in organ transplantation and forensic science․
1․1 Importance of ABO Blood Typing in Transfusion Medicine
ABO blood typing is critical for ensuring safe blood transfusions, preventing adverse reactions, and maintaining patient safety․ It determines donor-recipient compatibility, minimizing risks of hemolytic reactions․ Accurate ABO typing is essential for avoiding life-threatening complications, making it a cornerstone in transfusion medicine․ Understanding ABO antigens and antibodies ensures proper blood product selection, safeguarding transfusion outcomes and improving patient care․
1․2 Brief Overview of the ABO Blood Group System
The ABO Blood Group System categorizes blood into four types (A, B, AB, O) based on A and B antigens on red blood cells․ Type A has A antigens, Type B has B antigens, Type AB has both, and Type O has neither․ This classification is crucial for safe blood transfusions, preventing immune reactions between donor and recipient blood․

Historical Background of the ABO Blood Group System
The ABO blood group system was first discovered by Karl Landsteiner in 1901, marking a pivotal moment in transfusion medicine and blood type classification․
2․1 Discovery and Classification of ABO Blood Groups
Karl Landsteiner identified the ABO blood groups in 1901 by observing agglutination reactions between red blood cells and sera․ This led to the classification of blood into four types: A, B, AB, and O, based on the presence or absence of A and B antigens, revolutionizing transfusion medicine and blood compatibility testing․
2․2 Evolution of Understanding ABO Antigens and Antibodies
Early studies by Landsteiner revealed ABO antigens, while later research clarified the role of anti-A and anti-B antibodies in blood compatibility․ Advances in genetics and immunology further defined the ABO system, showing how alleles A, B, and O determine antigen expression․ This knowledge has refined blood typing techniques and transfusion safety, ensuring compatible blood products for medical procedures․
The ABO Blood Group System
The ABO system classifies blood into four types (A, B, AB, O) based on the presence or absence of A and B antigens on red blood cells․
3․1 Structure and Function of ABO Antigens
ABO antigens are glycoproteins on red blood cell surfaces․ The A and B alleles produce enzymes adding specific sugars, forming A or B antigens․ These antigens determine blood type and trigger immune responses if incompatible blood is introduced, making them critical for transfusion compatibility and organ transplantation success․
3․2 Role of ABO Antibodies in Blood Compatibility
ABO antibodies are naturally occurring immune proteins that react with incompatible ABO antigens, causing agglutination․ They are crucial for determining blood compatibility in transfusions and organ transplants․ Individuals with type A blood have anti-B antibodies, while those with type B have anti-A antibodies․ Type O has both, and type AB has none․ This immune response ensures safe blood product matching and prevents adverse reactions․
3․3 Classification of ABO Blood Types (A, B, AB, O)
The ABO system classifies blood into four types: A, B, AB, and O․ Type A has A antigens and anti-B antibodies; Type B has B antigens and anti-A antibodies․ Type AB has both A and B antigens with no antibodies, while Type O has neither antigen but both antibodies․ This classification ensures safe blood transfusions and organ transplants by preventing immune reactions․
3․4 The Hh Blood Group System and Its Relation to ABO
The Hh blood group system regulates the synthesis of the H antigen, a precursor to A and B antigens․ Individuals with the hh genotype cannot produce H antigen, impacting ABO antigen expression․ This system influences ABO blood type classification, as the presence or absence of H antigen affects the strength of A and B antigens․ Blood types are ordered by H antigen levels: O, A2, B, A2B, A1, A1B․

Genetic Basis of the ABO Blood Group System
The ABO blood group system is determined by the ABO gene, which has three main alleles: A, B, and O․ These alleles determine blood type inheritance․
4․1 ABO Gene and Its Allelic Forms (A, B, O)
The ABO gene indirectly encodes the ABO blood group antigens․ The ABO locus has three main allelic forms: A, B, and O․ The A and B alleles each encode a specific enzyme responsible for producing A or B antigens, while the O allele does not produce any antigen․ These alleles determine the four main blood types: A, B, AB, and O․ This genetic variation is crucial for blood typing and compatibility in transfusions and transplants, as well as in forensic applications where blood group identification is necessary․ Understanding these allelic forms is essential for grasping the fundamental principles of the ABO blood group system and its implications in various medical and scientific fields․ Additionally, the inheritance patterns of these alleles follow Mendelian genetics, making it possible to predict blood types in families․ The structure and function of these alleles have been extensively studied to ensure safe blood transfusions and organ donations, highlighting the importance of genetic knowledge in transfusion medicine and beyond․
4․2 Inheritance Patterns of ABO Blood Groups
The ABO blood groups are inherited through alleles A, B, and O, following Mendelian genetics․ Each parent contributes one allele, resulting in possible combinations like AA, AO, BB, BO, AB, or OO․ These combinations determine the four blood types: A, B, AB, and O․ For example, inheriting A from one parent and B from another results in AB blood type, while inheriting O from both parents results in type O․ Understanding these inheritance patterns is crucial for predicting blood types in families and ensuring compatibility in medical procedures like blood transfusions and organ transplants․ This genetic knowledge also aids in forensic applications and personalized medicine, making it a cornerstone of transfusion science and genetics․ Accurate prediction of blood types relies on understanding how these alleles interact and express themselves across generations, ensuring safe and effective medical practices․
Blood Typing and Testing Methods
This section covers various methods for determining ABO and Rh blood types, ensuring compatibility in transfusions and transplants, vital for patient safety and care․
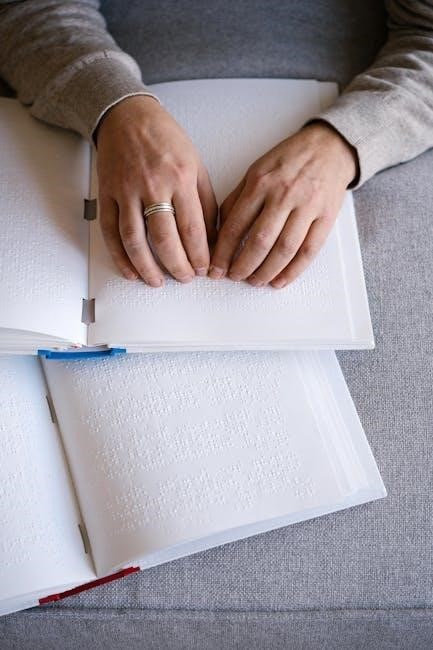
5․1 ABO Blood Typing Techniques
ABO blood typing involves testing red blood cells for A and B antigens using anti-A and anti-B sera․ Agglutination indicates the presence of specific antigens, determining blood type as A, B, AB, or O․ This method ensures accurate blood group identification, essential for safe transfusions and compatibility assessments․ It is a fundamental procedure in transfusion medicine and clinical diagnostics․
5․2 Rh Blood Type and Its Significance
The Rh blood type system involves the presence or absence of the Rh antigen on red blood cells․ Individuals are classified as Rh-positive (Rh+) or Rh-negative (Rh-)․ Rh compatibility is critical in blood transfusions and pregnancy, as Rh incompatibility can lead to adverse reactions․ The Rh system, alongside ABO, ensures safe blood product matching and prevents alloimmunization, making it vital in transfusion medicine and maternal healthcare․
Blood Product Compatibility and Transfusion Guidelines
Blood product compatibility is determined by ABO and Rh systems, ensuring safe transfusions․ Proper donor-recipient matching prevents adverse reactions, making it critical for patient care and outcomes․
6․1 Blood Donation and Recipient Compatibility
Blood donation and recipient compatibility are determined by ABO and Rh blood group systems․ Donors with type O negative are universal donors, while AB positive individuals are universal recipients․ ABO compatibility ensures safe transfusions, preventing adverse reactions; Plasma compatibility is also crucial, as ABO antibodies in plasma can affect recipient safety․ Proper matching of blood types minimizes risks and ensures optimal outcomes for patients receiving blood products․
6․2 Safe Blood Transfusion Practices
Safe blood transfusion practices rely on precise ABO and Rh compatibility testing to prevent adverse reactions․ Pre-transfusion testing ensures donor and recipient blood compatibility․ Proper identification of blood units and patients is critical․ Healthcare staff must be trained in blood handling and administration․ Continuous monitoring during and after transfusion helps identify and manage potential complications promptly, ensuring patient safety and optimal clinical outcomes․
Clinical Relevance of ABO Blood Groups
The ABO blood group system plays a critical role in transfusion medicine, organ transplantation, and forensic science, ensuring compatibility and preventing adverse reactions in clinical settings․
7․1 ABO Incompatibility in Transfusion Medicine
ABO incompatibility is a critical issue in transfusion medicine, occurring when donor and recipient blood types do not align, triggering an immune response․ This can lead to severe complications, including hemolysis, kidney failure, and even death․ Proper blood typing and cross-matching are essential to prevent such reactions, ensuring safe transfusions and maintaining patient health․
- ABO incompatibility can cause immediate adverse reactions․
- Pre-transfusion testing is vital to avoid antigen-antibody conflicts․
- Understanding ABO antigens is key to preventing transfusion errors․
7․2 ABO Considerations in Organ Transplantation
ABO compatibility is crucial for successful organ transplantation, as mismatched blood types can lead to graft rejection or failure․ Donor and recipient ABO blood groups must align to prevent immune-mediated complications․ ABO antigens on organ cells can trigger antibody responses, necessitating careful matching to ensure transplant viability and long-term success․
- ABO blood types influence organ compatibility․
- Matching donor and recipient blood groups reduces rejection risk․
- ABO antigens play a key role in transplant outcomes․
7․3 Forensic Applications of ABO Blood Grouping
ABO blood grouping is a valuable tool in forensic science, aiding in crime scene investigations and legal cases․ It helps identify blood stains and determine individual blood types, providing critical evidence․ This system is also used in paternity testing and resolving legal disputes, making it indispensable in forensic medicine for establishing identity and solving crimes․
- Identifies blood stains at crime scenes․
- Used in paternity and legal disputes․
- Provides critical forensic evidence․
Special Considerations in ABO Blood Typing
Special considerations include ABO subgroups like A2 and Bombay phenotype, which can affect compatibility․ These variations require careful typing to ensure safe transfusions and prevent adverse reactions․
8․1 ABO Subgroups and Their Implications
ABO subgroups, such as A1, A2, and A1B, exhibit variations in antigen strength․ These differences can affect blood compatibility and transfusion outcomes․ For instance, A2 individuals may have weaker A antigens, potentially impacting donor-recipient matching․ Additionally, rare subgroups like the Bombay phenotype lack the H antigen, complicating blood typing․ Understanding these variations is critical for ensuring safe transfusions and preventing adverse reactions in clinical settings․
8․2 ABO Incompatibility in Pregnancy
ABO incompatibility during pregnancy occurs when a mother’s immune system produces antibodies against the A or B antigens present on the baby’s red blood cells․ This can lead to hemolytic disease of the newborn, causing jaundice and anemia; Regular prenatal monitoring and timely interventions, such as intrauterine transfusions in severe cases, are essential to ensure a healthy outcome for the baby․
Modern Advancements in ABO Blood Group Research
Recent advancements focus on developing faster, accurate blood typing technologies and exploring the role of ABO antigens in disease resistance and personalized medicine․
9․1 Emerging Technologies in Blood Typing
Emerging technologies in blood typing include portable diagnostic devices and advanced serological assays․ These innovations enable rapid, accurate blood group identification, reducing errors in transfusion medicine․ AI-driven systems are being explored to enhance blood typing efficiency․ Additionally, next-generation sequencing offers deeper insights into ABO gene variations, improving personalized medicine approaches․ These advancements aim to revolutionize blood compatibility testing, ensuring safer transfusions and better patient outcomes globally․
9․2 Future Directions in ABO Blood Group Studies
Future research in ABO blood groups focuses on advancing genomics and epigenetics to better understand antigen variability․ AI-driven predictive models may enhance blood type matching for transfusions and transplants․ Exploring the role of ABO in disease susceptibility and immune responses is another key area․ Additionally, global standardization of blood typing protocols and ethical considerations in personalized medicine will shape the future of ABO blood group studies, ensuring safer and more tailored healthcare solutions․
